X-Ray Irradiation for Virus Inactivation
X-ray Irradiation for Virus Inactivation
X-ray irradiation has become a crucial tool for virus inactivation, balancing effective pathogenneutralization with or without the preservation of viral structural integrity. This technique is widelyemployed in virology for applications such as vaccine development, diagnostic research, and the safehandling of pathogenic samples.
The significance of X-ray irradiation is underscored by its ability to inactivate viruses with or withoutcompromising their biochemical and immunological characteristics. Research has demonstrated thatoptimized X-ray doses effectively inactivate zoonotic RNA viruses, such as Zika, Hazara, Bebaru, and RiftValley Fever (Afrough, et al, 2020). Moreover, X-ray irradiation facilitates the safe transfer and analysis ofinactivated viruses in laboratories with lower biosafety levels.
Classification of Viral Resistance to Irradiation
Viruses exhibit varying degrees of resistance to ionizing radiation, primarily influenced by their genomiccomposition and structural complexity:
- High Resistance: Prion diseases such as kuru, Creutzfeldt-Jakob disease, and scrapie exhibitextreme resistance to ionizing radiation. Even high doses (up to 200 kGy) have shown minimalreduction in viral titers, suggesting a unique structure compared to other mammalian viruses.
- Moderate Resistance: Non-enveloped viruses, including adenoviruses and parvoviruses,demonstrate moderate resistance due to their robust capsid structures.
- Low Resistance: Enveloped viruses such as influenza and herpesviruses are more susceptible toirradiation, as their lipid envelopes are prone to damage.
Applications of X-ray Irradiation in Virology (Figure 1)
X-ray irradiation serves multiple critical functions in virology, including:
1. Complete Inactivation for Safety: Ensuring complete virus inactivation is essential for safehandling and study. X-ray irradiation has been used to inactivate high-consequence pathogens,such as Ebola and Lassa viruses, making them safer for research in standard laboratory conditions.
2. Facilitating Research in Lower Biosafety Laboratories: Inactivating viruses enables their safetransfer to lower biosafety-level labs, reducing the need for high-containment facilities whileallowing broader research access .
3. Studying Viral Pathways: X-ray irradiation allows researchers to investigate viral entrymechanisms, replication processes, and interactions with host cells without infection risks.
4. Sequencing and Genomic Studies: By inactivating viruses, irradiation enables safe viral nucleicacid extraction and sequencing, aiding genomic research and the development of molecular diagnostics.
5. Vaccine Development: X-ray irradiation is used to inactivate viruses while preserving theirimmunogenicity, which is essential for developing vaccines that induce strong immune responseswithout causing disease.
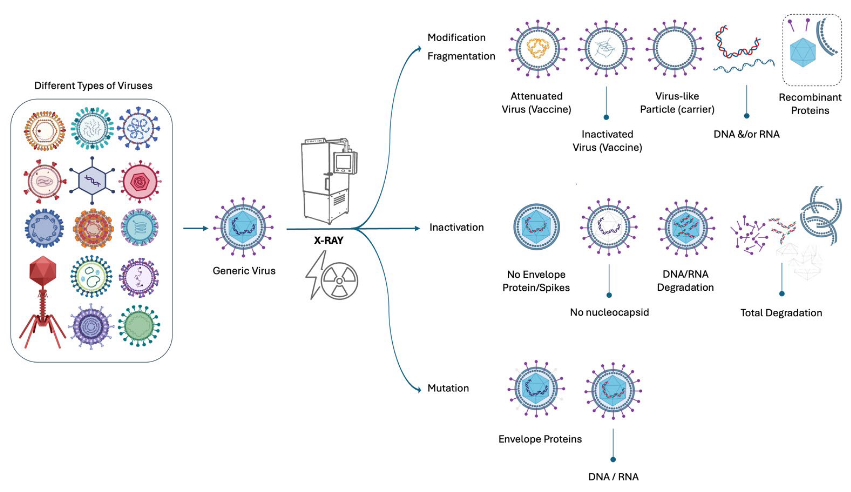
Figure 1. Applications of X-ray Irradiation in Virology.
Virus Inactivation Research Utilizing Precision X-Ray, Inc. Systems
Precision X-Ray, Inc. systems have been instrumental in virology research, providing precise and reliableirradiation capabilities. As an example, Afrough et al (2020) at the National Infection Service, the Centrefor Chemical, Radiation and Environmental Hazards at Public Health England, and the CBR Division,Defense and Science Technology Laboratories in England, utilized a MultiRad 225 to explore X-rayinactivation of RNA viruses without loss of biological characteristics.
This study defines the amount and type of X-ray radiation needed to create replication-deficient versionsof several viruses while maintaining their key biochemical and immunological properties. These virusescan then be used in detection and functional assays, offering a reliable way to produce non-infectiousreagents for diagnostics and R&D in lower containment labs.
The results showed that X-ray inactivation can be effectively achieved for a range of medically import antzoonotic viruses. X-ray irradiation is a reliable method for pathogen inactivation, allowing the production of non-infectious whole-virus material that retains its key biochemical and immunological properties under standard inactivation conditions. These findings provide a unique tool for quickly develop in greagents for various downstream applications in a safe and reproducible way.
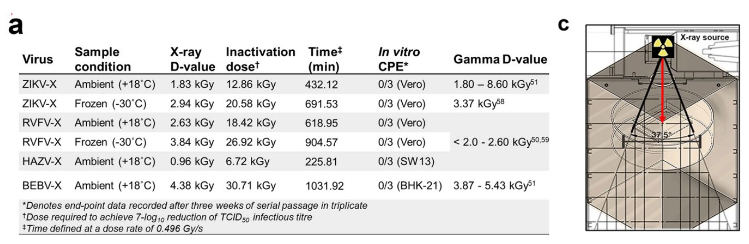
a. Inactivation of viral pathogens using X-rays. X-ray D-values showing the dose required to inactivate 1-log10 of virus at 220 keV, 17.5 mA with 0.2 mm Al filtration. X-ray D-values were then compared togamma inactivation data produced under similar sample conditions, for members of the same genus. c.Effect of X-ray beam filtration on ZIKV inactivation. The irradiation chamber showing the sealed virusspecimens with packaging dimensions of 10 cm × 8 cm × 1 cm (L x W x D) at a distance of 22.6 cm withina 37.5° irradiation cone produced by the MXR-225/26 tube. Adapted from: Afrough, et al. (2020).
Conclusion
X-ray irradiation remains a versatile and effective tool in virology, enabling the safe and efficientinactivation of viruses. Its applications range from vaccine development to fundamental virology research,contributing significantly to public health and scientific advancement. Precision X-Ray, Inc. systems suchas the X-RAD 320 or MultiRad 225 continue to play a crucial role in advancing virological studies byproviding precise irradiation capabilities for a variety of research applications.
References
- Afrough B, Eakins J, Durley-White S, Dowall S, Findlay-Wilson S, Graham V, Lewandowski K, CarterDP, Hewson R. X-ray inactivation of RNA viruses without loss of biological characteristics. Sci Rep.2020 Dec 8;10(1):21431
- Darnell, M. E. R., Taylor, D. R., & Bird, B. H. (2004). Inactivation of the SARS coronavirus by gammairradiation. Emerging Infectious Diseases, 10(3), 552-555.
- Kremer, J. R., Wrigley, N. G., & Brown, A. (2019). Safe handling of viral samples: X-ray irradiationand biosafety considerations. Journal of Virology Methods, 265, 23-30.
- Campbell, E., Afrough, B., Bonney, L., Curran-French, M., Chamberlain, J., Daddiego, J., … &Hewson, R. (2024). X-ray Inactivation of SARS-CoV-2: A Safe, Cost-effective Approach forPandemic Testing Workflows.
- Eakins, J. S., Afrough, B., & Hewson, R. (2021). Monte Carlo modelling of an x-ray chamber forproviding inactivation exposures to viruses. Journal of radiological protection, 41(4), 962.
- Lee, A. K., Pan, D., Bao, X., Hu, M., Li, F., & Li, C.Y. (2020). Endogenous retrovirus activation as akey mechanism of anti-tumor immune response in radiotherapy. Radiation research, 193(4), 305-317.
- Liu KK, Shan CX. Viral inactivation by irradiation rays. Light Sci Appl. 2023 Mar 14;12(1):72. doi:10.1038/s41377-023-01108-3.
